Respiratory infections are very common infections in kids as well as adults. We know that respiratory tract infections are usually due to lower immunity response. Type 1 diabetes increases the tendency for both chronic and acute infections by weakening the immune mechanisms. The risk is specifically increased for respiratory tract infections, along with other infections have also been associated with diabetes. Study was conducted where investigation was carried out whether viral respiratory tract infections in children with type 1 diabetes might impose an additional burden on the arterial endothelial function or not.
As per the study, Upper-respiratory infections in early childhood and especially in the first year of life is associated with an increased risk for type 1 Diabetes Mellitus.
Epidemiology:
The incidence of diabetes mellitus is increasing rapidly in India as well as abroad. In addition to well-known other complications, diabetes increases the risk for hospitalization and death from severe acute respiratory infection (SARI) and influenza, pneumonia and tuberculosis. Male are more affected than females. Older groups are more prone to respiratory tract infections than younger groups.
Pathophysiology:
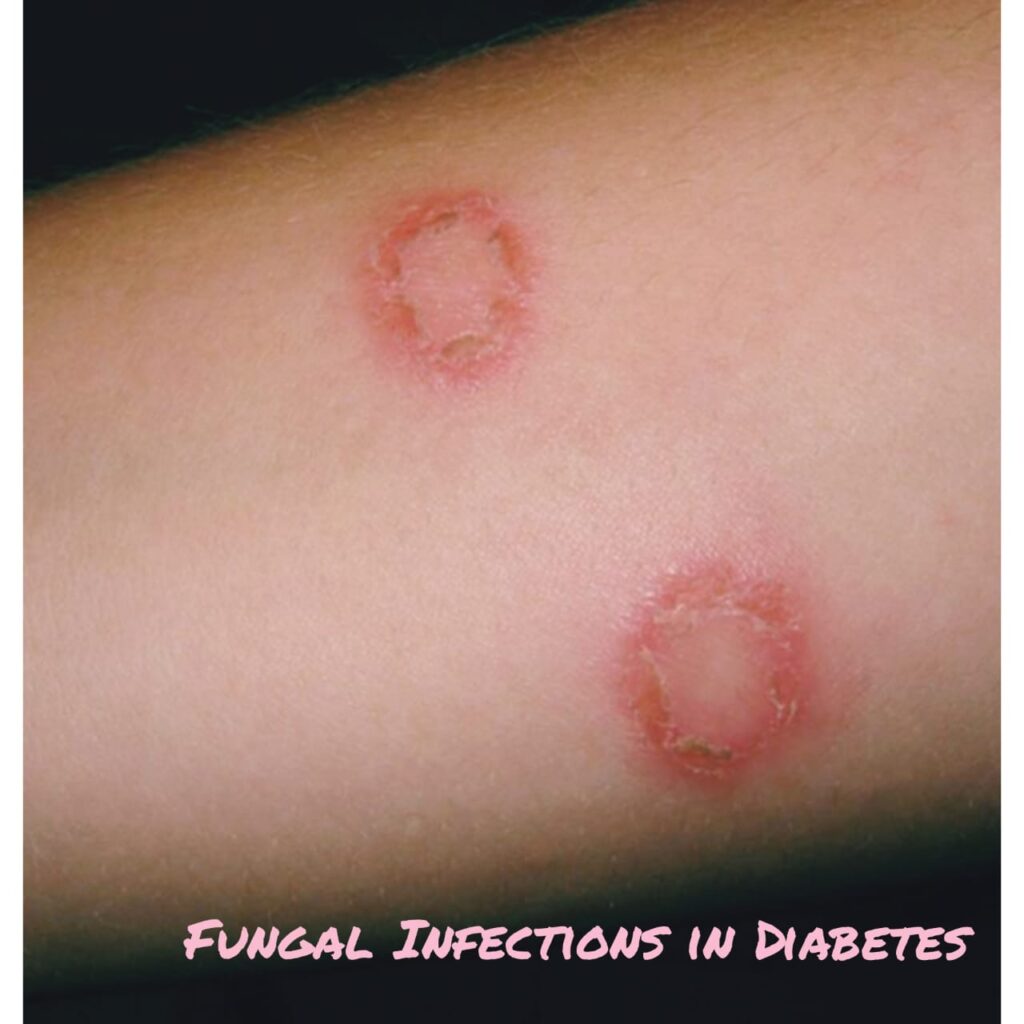
Diabetes increases the susceptibility to get different kinds of respiratory infections, which is usually identified as an solo risk factor for developing lower respiratory tract infections. Pulmonary infections caused by staphylococcus aureus, Mycobacterium tuberculosis, gram-negative bacteria and fungi may occur with an increased frequency, whereas infections due to influenza virus or Streptococcus pneumonia may be associated with increased mortality and morbidity.
During lung infection, there are changes in the ciliary epithelial lining. Increased susceptibility to pneumococcal infection by individuals with diabetes is due to reduced defense capability of antibodies to protein antigens. The incidence of tuberculosis in diabetic individuals is 5-6 times greater than among the non-diabetic population. It is observed that the malfunction of monocytes in patients with diabetes may contribute to the increased susceptibility to tuberculosis with a worse prognosis. Hospitalization of patients with diabetes due to influenza virus or flu-like infections is up to 7 times more likely to occur compared to healthy individuals, also diabetic patients are more likely to be hospitalized due to infection complications.
Signs and Symptoms:
- Breathlessness
- Wet Cough and cold, running nose in case of upper respiratory infections.
- Fever
- Loss of weight
- Weakness
- Bodyache, headache
- Itching of the body
- Thirst for sips of water
Investigation and Diagnosis:
- CBC
- ESR
- X ray chest PA view
- Blood sugar levels both fasting and Post pariandal
- CT scan chest for extent of pneumonia
- Chest pain
- Sputum examination for bacteria
- Mantoux test to rule out tuberculosis.
Management:
Immunization with influenza and anti-pneumococcal vaccines is the usual mode of treatment recommended to reduce hospitalizations, medical expenses and deaths. Also Diabetes should be monitored on regular basis. Antibiotics should be administered along with antitussives for upper respiratory tract infections like cold and cough with throat infections. Home remedies should be advised like warm water with lemon, steam inhalation for boosting immunity. Plate diet should be advised for Diabetes. Also one should consult a diabetologist for regular monitoring of blood sugar levels. Breathing exercises like yoga are very beneficial for healthy lifestyle.