Is diabetes affecting your eyes?
Introduction
People with diabetes may experience a variety of eye issues, collectively called “diabetic eyes.” These include glaucoma, cataracts, diabetic retinopathy, and diabetic macular edema.
Diabetes is essentially a metabolic disorder. The body is not processing the food that you eat correctly. A hormone called insulin delivers glucose to the cells in your body. In diabetes, either the body does not produce enough insulin or the cells are just resistant to it.
The blood vessels and neurons, including the ones in your eyes, get damaged when there is too much glucose in the blood rather than inside the cells. This eventually causes poor vision or even blindness. However, by managing diabetes, you can take measures to stop this progression.
How do you know if diabetes is affecting your eyes?
- Brief episodes of blurred vision:
High glucose levels in the blood alter the fluid quantity inside the eye, leading to swelling and causing blurred vision. This kind of hazy vision is transient and goes away as your blood sugar levels return to normal.
- Persistently high blood sugar
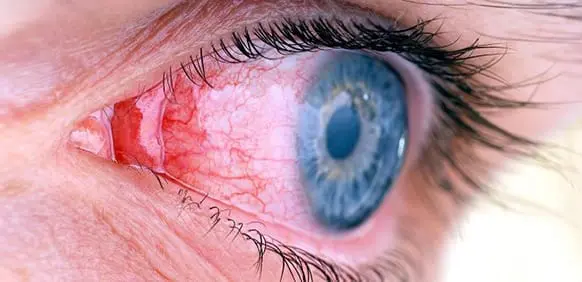
This can harm the tiny blood vessels behind your eyes. The damaged blood vessels leak to cause swelling. They eventually rupture and cause bleeding into the center of the eye increasing the eye pressure.
Diabetic eyes and their types:
Diabetic retinopathy
The retina is a structure at the back of the eye. It is the light-absorbing center. Diabetic retinopathy is a condition where the retina is harmed by the surrounding damaged blood vessels.
Blood sugar ruins the health of the blood vessels, leading to leakage into the retina in early diabetic retinopathy.
As the illness progresses, some blocked capillaries stimulate the growth of newer, frail blood vessels. This causes serious vision issues. Diabetic retinopathy is fairly common. Early diagnosis and management of diabetic retinopathy can significantly lower the risk of blindness—by 95%.
Diabetic macular edema
The macula is that part of the retina that helps in clear vision. Leakage from the capillaries causes macular edema, or swelling. Blindness or partial vision loss may eventually ensue. Macular edema is the aftermath of diabetic retinopathy.
Glaucoma
Diabetes is a contributing factor to a certain type of glaucoma. Leakage and overgrowth of the blood capillaries near the iris (the colored part of the eye) raise eye pressure to abnormal levels, leading to glaucoma.
Swelling of the eye lens
A sudden rise or fall in blood sugar alters the shape of the delicate lens in the eyes. This results in blurry vision. The vision goes back to normal after your blood sugar stabilizes.
Cataract:
People with diabetes may develop cataracts at an early age; the progression of the cataract is also rapid when blood sugar levels are high. This causes a cloudy buildup in the lens of the eye, and blurred vision.
Can you have diabetes-related eye disorders?
The incidence of eye problems caused by diabetes increases in the following scenarios:
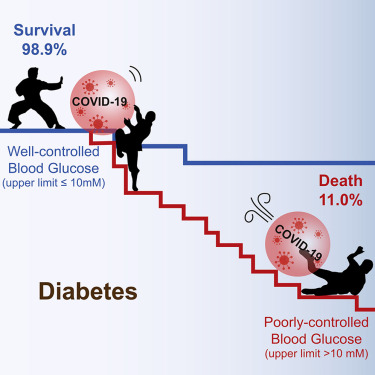
- Uncontrolled blood sugar levels
- Persistent high blood pressure
- High blood cholesterol levels.
- Smoking
- Comorbidities
Early-stage diabetes eyes symptoms
Initially, diabetes-related eye disorders show no signs. Gradually, you may begin to notice a few things:
- unsteady or blurred vision
- poor color perception
- flashing lights
- dim areas or reduced vision
- Frequent vision fluctuations, sometimes even daily.
- spots or strings of darkness (also known as floaters)
There are diabetic eye-related medical emergencies that warrant an immediate phone call to your diabetologist. This includes:
- A feeling of a sudden cover over the eyes (blurring)
- Rapid flashes of light floaters that remain constant for more than a day.
These could be signs of the retina losing its attachment. Call your doctor immediately.
Eye checkups in diabetes:
If you have diabetes, you need to get your eyes checked periodically.
- You will be given an eye drop in the clinic to enlarge the pupil and have better visual access to the retina.
- Pictures of the backs of the eyes are taken using a specialized camera.
In-built AI apps are available these days that can read the results of the retinal examination to diagnose diabetic eyes.
Diabetes eye treatment:
- Treat diabetes at its source by implementing the ABCs schedule, which includes quitting smoking and routine monitoring of HbA1c, blood pressure, and cholesterol.
- In terms of medical treatment, VEGF-blocking medications are the mainstay. These can stop fluid leaks and inhibit the growth of abnormal blood vessels in the eye.
- With a laser beam, also known as photocoagulation, small burns are made inside the eye. This procedure addresses internal swelling and blood vessel leakage.
- Vitrectomy is the surgical way to remove the vitreous humor or the fluid that fills the inside of the eye. The procedure treats problems with severe bleeding to prevent the formation of diabetic retinopathy.
- In the case of cataracts, the cloudy lens is removed and an artificial lens is placed.
How to prevent eye damage from diabetes
Golden rule: Manage the blood sugar levels first!
Check your blood sugar after short breaks or use a continuous glucose meter. You might need to check it more frequently if you are anxious or ill. Provide yourself with a target sugar level and work towards it. 85-140 mg/dL before food and less than 185 mg/dL 1-2 hours after meals are good.
Apart from that,
- Maintain healthy cholesterol and blood pressure levels (regular monitoring and medications). Reduce salt consumption. Low-salt diets also assist in maintaining the health of your eyes by reducing inflammation in the tiny blood vessels there. Use pink salt or other herbs to flavor.
- Avoid smoking. Nicotine patches and e-cigarettes come in handy.
- Exercise walks, or workouts should become routine. Moderate-intensity exercises like brisk walking are mandatory. Use workout gadgets like smart watches and pedometers to gauge your progress. Find enjoyable exercises to motivate yourself like Zumba.
- Include face yoga and eye exercises. It is a great way of destressing yourself.
- Plenty of fruits and vegetables should be included in your daily diet. To help prevent retinopathy, consume fresh fruit, vegetables, and fish. Obesity increases your risk of developing diabetic eye conditions. Simple homemade food and zero junk food can do wonders.
- Protect the eyes from UV rays and too much screen time. Use appropriate eyewear for the same.
Conclusion:
Periodic screening of the abdomen is vital in today’s world. High levels of blood sugar could be warning signs for other underlying disorders, like pancreatic cancer.