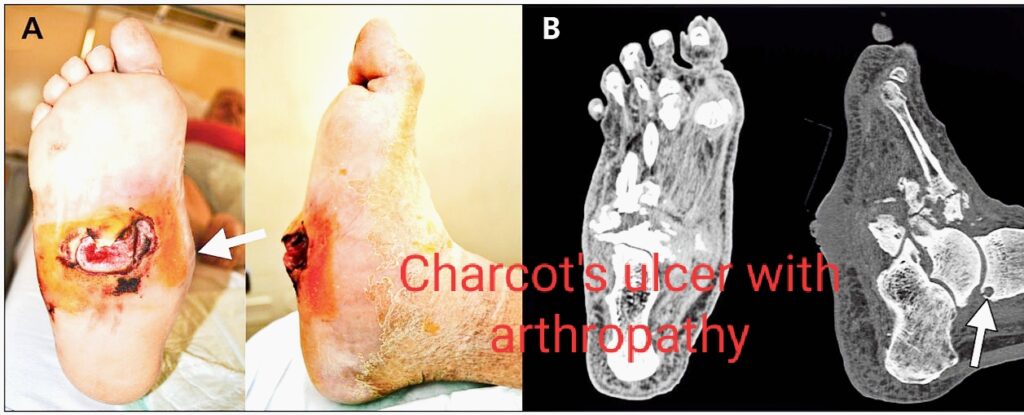
Charcot foot is a serious complication with people suffering from diabetes. The patient suffers from peripheral neuropathy along with diabetes. It affects the bones, joints and deeper soft tissues of foot and ankle. The bones become weak and fragile and ankle can easily dislocate. Charcot’s foot is also known as Charcot’s arthropathy. When the midfoot is involved in this, the arch of the foot collapses, which curls around the bottom of the foot. This is known as rocker-bottom foot deformity.
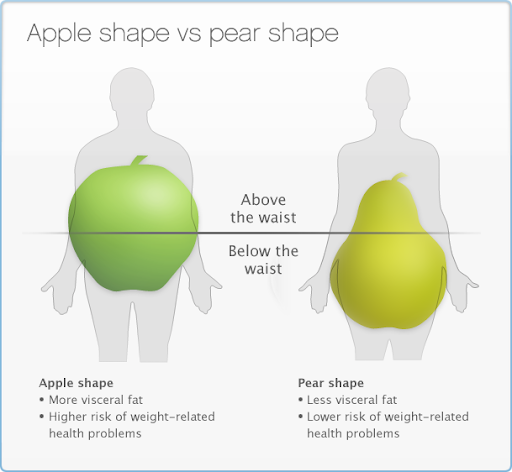
Charcot Foot’s known cause is Diabetic Neuropathy. Due to foot deformities, there is abnormal pressure on the plantar surface of the foot which lead to foot ulcers. This in turn leads to nerve damage and there is loss of sensation, unilateral swelling and erythema of the foot. When the patient is suffering from diabetes, the foot ulcers pose a high risk for amputation of foot. Hence one needs to be cautious for any injury, frostbite etc. Obesity can also lead to pressure over the foot. There may be slight pain if the sensory loss is not complete. However one can misjudge the diagnosis for cellulitis. The bones of the foot slowly begin to lose calcium which makes the bones strong.
Charcot Foot Causes:
- Alcohol/drug abuse
- Spinal cord injury/disease
- HIV
- Parkinson’s disease
- Any infection
- Syphilis
- Injury to foot
- Sprain to ankle
- Any foot surgery very slow to heal
There is no specific cause for charcot’s foot. The above mentioned are the trigger factors for this disease.
Diagnosis:
Sometimes charcot’s foot can also mimic deep vein thrombosis. A venous duplex scan can help to rule out venous occlusion. X Ray of affected foot show bony destruction, joint subluxation, fragmentation and bony remodelling.
Charcot Foot Treatment:
Immobilisation of foot:
This protects the feet to move and create pressure. One can use crutches, wheelchair or a knee Walker to go around. One should rest for at least 2 months to avoid unnecessary pressure on the foot. Also offloading the foot, that is putting the foot into cast which protects the foot from bearing weight and helps in immobilisation. This cast is changed several times till the swelling of the foot goes down. Orthopedic footwear usually relieves pressure points and avoids ulcers and injury.
Repair bones with surgery:
Any injury to the foot can make your foot unstable, or you can’t wear special shoes or braces then surgery would help in such cases. Also in cases of sore foot, surgery is necessary.
Care your foot:
Focus on your foot. Make sure you go for regular checkups for diabetes. Look for signs like unilateral swelling, warm spots, redness, sores or ulcers. Check for any redness and sores in-between your toes. Wash your feet daily. Always wear your socks and shoes.
Treatment with antimicrobial medicines:
When the patient has lot of pain and swelling of the foot with accumulation of abscess leading to ulcer, then antimicrobials are the first choice of the physician.
When surgery is the only choice:
Surgery is adviced for those patients who have severe foot and ankle deformities endangering to foot ulcers. Amputation is done when foot ulcer worsens. Also Diabetes should be under complete check.
Complications:
When the patient suffers from deformity of ankle, the joint may become unstable or “floppy” due to replacement of the tissue o er the bone joint. This “floppy foot” can lead to ulcers. Foot ulcers are difficult to heal due to uncontrolled Diabetes, which leads to poor circulation in feet, leading to Infections. This condition can be threatening causing amputation of foot depending upon the extent of infection.
If you like this article, Share with your friends.