Chai Time on a Rainy Day: Is Tea Good for Diabetes?
Table of Contents
- ● Introduction
- ● Types of Tea
- ● Benefits of Tea for Diabetics
- ● Be a Safe Tea Drinker if You Have Diabetes
- ● Conclusion
Introduction
Life may throw storms our way, but during chai time, we find solace, warmth, and the strength to face whatever comes next.
Rainy days and chai go hand in hand, creating the perfect symphony of tranquility and warmth. It is the perfect blend of flavors, like friendships, it brings joy and sweetness to our lives. Tea is one of the most widely consumed beverages in the world, including in India, where it holds significant cultural importance. Chai time, is cherished by many; whether it be a rainy day or a work break, a cup of hot tea is always welcome. Knowing how tea affects the blood sugar levels is important for diabetics. This article will delve deeper into the relationship between tea and diabetes, considering its potential benefits, and factors to consider.
Types of Tea:
Tea comes in various forms, with black, green, and herbal tea being the most popular options.
Each type of tea undergoes different processing methods, resulting in variations in taste, aroma,
and health benefits.
● Black Tea
Black tea is the most common type of tea consumed in India. It is fully fermented and has a stronger flavor compared to other teas. Black tea contains compounds called theaflavins, catechins, and thearubigins, which have antioxidant properties.
● Green Tea
Green tea is known for its minimal processing, which helps to retain its natural antioxidants, such as catechins. Catechins are believed to have potential health benefits, including antioxidant and anti-inflammatory properties.
● Herbal Tea
Herbal teas are made from various plants, flowers, and herbs. Popular options in India include tulsi (holy basil), ginger, cinnamon, and chamomile. Herbal teas are caffeine-free and often have distinct medicinal properties associated with their ingredients.
The Benefits of Tea for Diabetics
People with diabetes may benefit from drinking tea, especially certain varieties like herbal and green teas.
Here are some of the potential benefits of tea for diabetes:
● Antioxidant Properties
Antioxidants called polyphenols (catechins) found in tea, particularly green tea, help shield the
body’s cells from oxidative stress-related cell damage. Oxidative stress is often higher in individuals with diabetes and can contribute to the development of complications. Antioxidants in tea may help reduce oxidative stress and promote overall health.
● Blood Sugar Control
Some studies suggest that certain compounds found in tea, such as catechins in green tea, may help improve blood sugar control. These compounds may enhance insulin sensitivity, promote glucose uptake in cells, and inhibit glucose absorption in the digestive system. As a result, tea consumption may contribute to better management of blood sugar levels.
● Improved Insulin Sensitivity
Research indicates that tea consumption, particularly green tea, may improve insulin sensitivity. Insulin sensitivity refers to the body’s ability to respond effectively to the hormone insulin, which regulates blood sugar levels. By enhancing insulin sensitivity, tea may support better glucose control and reduce the risk of insulin resistance, a common feature of type 2 diabetes.
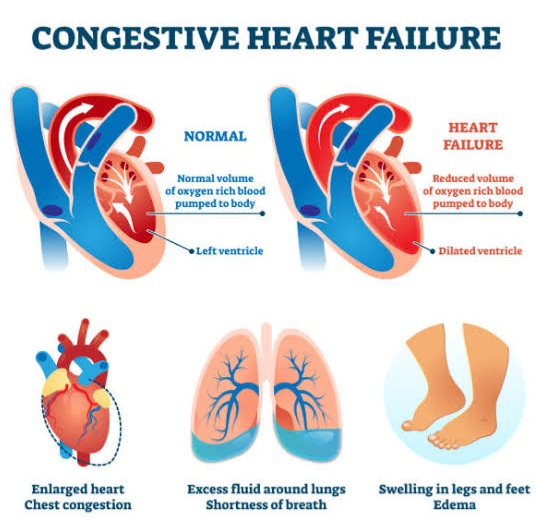
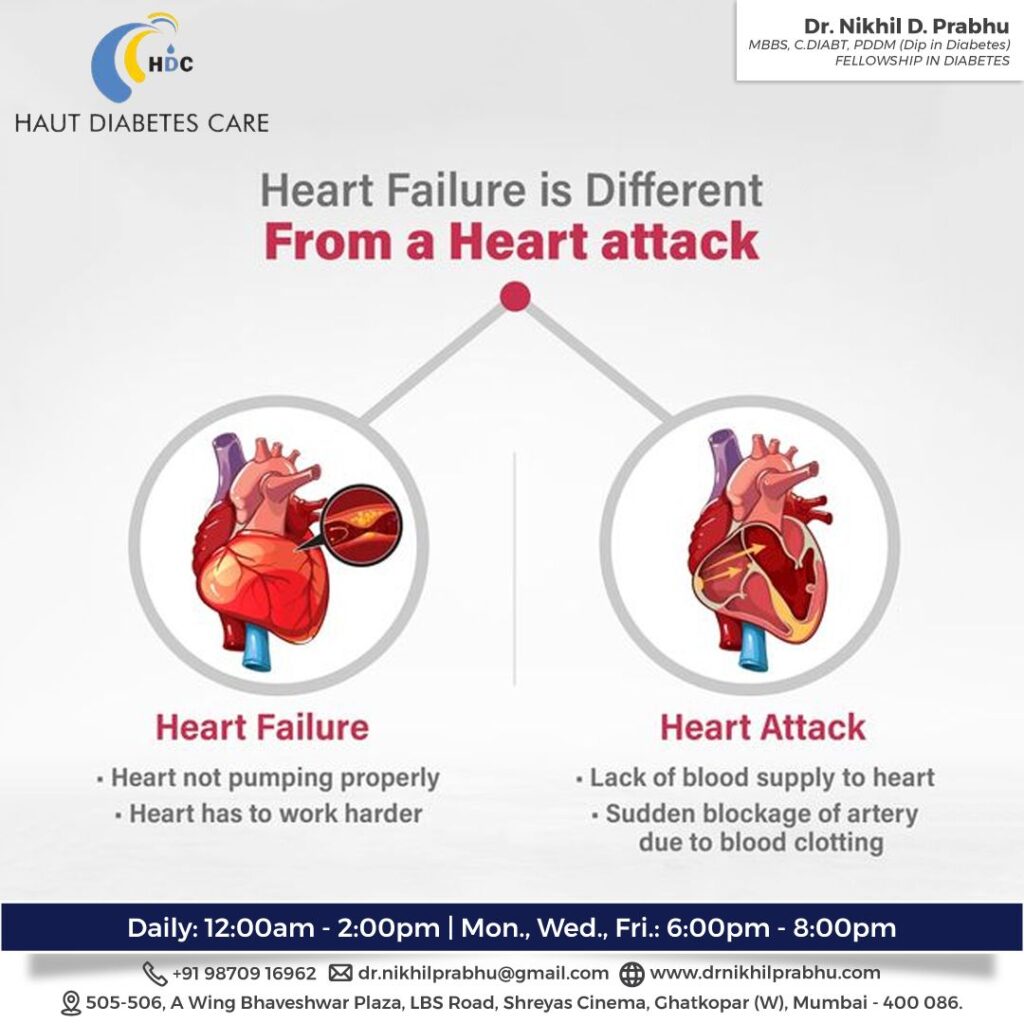
● Cardiovascular Health
People who have diabetes are more likely to get cardiovascular diseases. Regular tea consumption, especially green and black teas, has been associated with a reduced risk of heart disease and stroke. Tea’s potential cardiovascular benefits include improving blood pressure, reducing LDL (bad) cholesterol levels, and enhancing blood vessel function.
● Weight Management
To effectively manage diabetes, one must maintain a healthy weight. Tea, particularly green tea, may support weight loss and weight management efforts. It contains catechins and caffeine that have been shown to boost metabolism and increase fat oxidation. Incorporating tea into a balanced diet and exercise regimen may help with weight control.
● Stress Reduction
Stress can affect blood sugar levels and overall diabetes management. Tea, especially herbal teas like chamomile and lavender, has calming properties that can help reduce stress and promote relaxation. By managing stress levels, individuals with diabetes may experience improved blood sugar control.
It’s important to note that while tea may offer potential benefits for diabetes management, it is not a substitute for medical treatment, a healthy diet, regular exercise, and prescribed medications.
Be a Safe Tea Drinker if You Have Diabetes
While tea can have potential benefits for individuals with diabetes, it’s essential to consider the following factors:
● Frequency
Overconsumption of anything is bad, and tea is no different. Tea addiction can cause other potential side effects, like tooth stains and gastric issues.
● Caffeine Content
Tea naturally contains caffeine, which can affect blood sugar levels in some individuals. It’s advisable to monitor your response to caffeine and consult with your healthcare provider or diabetologist to determine the right amount of tea consumption for you.
● Sugar and Sweeteners
Be cautious of adding sugar or sweeteners to your tea, as these can significantly increase the carbohydrate and calorie content. Opt for natural alternatives like stevia or enjoy tea without any additional sweeteners.
● Pair Tea with Balanced Snacks
When enjoying a cup of tea, consider pairing it with diabetes-friendly snacks that provide a balance of nutrients. This can help prevent rapid blood sugar spikes and promote better glycemic control.
● Medication Interactions
If you are taking diabetes medications, it's crucial to be aware of any potential interactions between tea and your medications. Certain compounds in tea may affect the metabolism of medications, so consult your healthcare provider to understand any potential risks or adjustments needed.
Conclusion
With every sip of chai, we taste the essence of tradition, culture, and the rich heritage that brings us together. However, with diabetes, consume chai in limited quantities and only the sugar-less, organic ones. By incorporating tea into your diabetes management plan thoughtfully, you can enjoy the warmth and comfort of a cup of tea on a wet rainy day, while supporting your overall health and well-being. So, grab your favorite mug, savor the aroma, and enjoy a moment of tranquility during chai time on a rainy day while keeping your diabetes management on track.