Diabetes is a global disease and it is predicted that it will be affecting over 80 million individuals by 2025 in India and over 300 millions around the world. Compared to the disease progression, its awareness is very low among Indian population. Even though diabetes is common, many people don’t know much about it – this includes people who are at greatest risk.
Here are 10 myths and facts about diabetes.
Myth 1 : Diabetes is caused by eating too much of sugar
Fact 1 – Diabetes is not caused by eating too much of sugar. There are 2 types of diabetes i.e Type 1 diabetes and Type 2 diabetes. In Type 1 diabetes (Juvenile Diabetes), body doesn’t produce hormone, called insulin, which manages blood sugar levels. The exact cause of Type 1 diabetes is unknown. But it is believed that autoimmunity, genetics and environmental factors like certain viral infections plays an important role in its etiology.
In Type 2 diabetes body produces insulin hormone, but either it is less in quantity or its action is impaired (insulin resistance) and not able to maintain blood sugar level at normal levels. Abdominal obesity (tummy fat) is believed to be culprit for insulin resistance, in Indian population.
Other causes of diabetes includes excessive alcohol consumption which lead to repeated pancreatitis and ultimately beta cell destruction of pancreas leading to insulin shortage and diabetes. Certain pancreatic surgeries like surgery for cancer of pancreas involving tail part or removing entire pancreas lead to insulin deprivation and diabetes.
Myth 2 : Diabetic person should not eat chocolates, sweets, etc
Fact 2 – Diabetic people can eat chocolates, sweets etc BUT they have to limit the quantity at each serving. Diabetes management is an art of balancing blood sugar level. Foods with low glycemic index raises blood sugar level but to a lower extent whereas those with high glycemic index raises blood sugar level rapidly. Mild to moderate exercise like walking, cycling etc helps to lower blood sugar level. No food is absolutely forbidden if you can maintain the consumption of proper portion size.
Myth 3 : If you are overweight or obese then you will get diabetes for sure.
Fact 3 – Every overweight or obese individual may not get diabetes. There are several other factors such as family history, etc. which are also contributory. But ofcourse, obesity (especially abdominal obesity) is an important risk factor for insulin resistance and diabetes. You can see all other risk factors for diabetes in my previous article.
Myth 4 : Once insulin started it will remain life long.
Fact 4 – No, not always. Insulin can be of best choice in certain conditions like prior to operation or surgeries, in acute infections or stress, certain conditions where oral intake of food is limited etc. Insulin can be given temporary in these conditions as insulin helps in wound healing. It has very less chance of interaction with other medicines.
Diabetes is progressive disease. Almost 50% of beta cells are dead when diabetes detected for first time. Over the years beta cells keep on decreasing with use of sulfonylurea drugs. Eventually a stage comes, after around 7-10 years, when there is very less beta cell reserve to produce insulin. At this stage patient requires external insulin injections. Around 25% of Type 2 diabetes patients reach beta cell exhaustion stage & require insulin.
Myth 5 : Diabetes is curable.
Fact 5 – No. There is no cure for diabetes till now. Diabetes can be well controlled with diet, exercise and timely proper medications.
In case of pre-diabetic stage, diabetes can be reversed or delayed. This can achieved by maintaining proper diet, and exercise to induce weight loss. Certain insulin sensitizers like metformin can also be used. But once you have established diabetes, it is not curable.
Myth 6 : Herbal supplements can reverse or cure diabetes.
Fact 6 – Once diabetes is confirmed, it is not curable with any herbal supplements and medicines. HbA1c (Glycated Hemoglobin) is most reliable blood test to confirm diabetes.
Myth 7 – Diabetes is contagious
Fact 7 – Diabetes is not contagious and not transmitted from person to person.
Myth 8 : Insulin injections are very painful
Fact 8 – No, insulin injections are not painful as the needle is very small and very thin compared to normal blood collection needles. Nowadays insulin flex pens are available for insulin injections, they are designed in such a way that patient can himself take insulin shot without any pain.
Myth 9 : Type 2 diabetes is only seen in adults
Fact 9 – Nowadays, Type 2 diabetes has also been observed in children as well. Type 2 diabetes has been detected in a 5 year old child. Faulty lifestyle, poor food habits and childhood obesity are the culprits for this.
Myth 10 : People with diabetes can’t live active healthy life
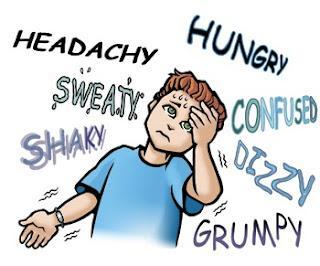
Fact 10 – No. Exercise, in the form of brisk walking or even cycling, lead to increase glucose uptake by muscles. Exercise also increases insulin sensitivity. Thus an active life along with exercise is very helpful for diabetes patient. Diabetic patients on insulin or certain drugs which increase insulin production from pancreas need to take special precautions like having a carbohydrate rich snack before exercise to prevent hypoglycemia.
Those were the top 10 myths and facts about diabetes. If you like my article please share it with your friends and family.
Awareness is prevention !