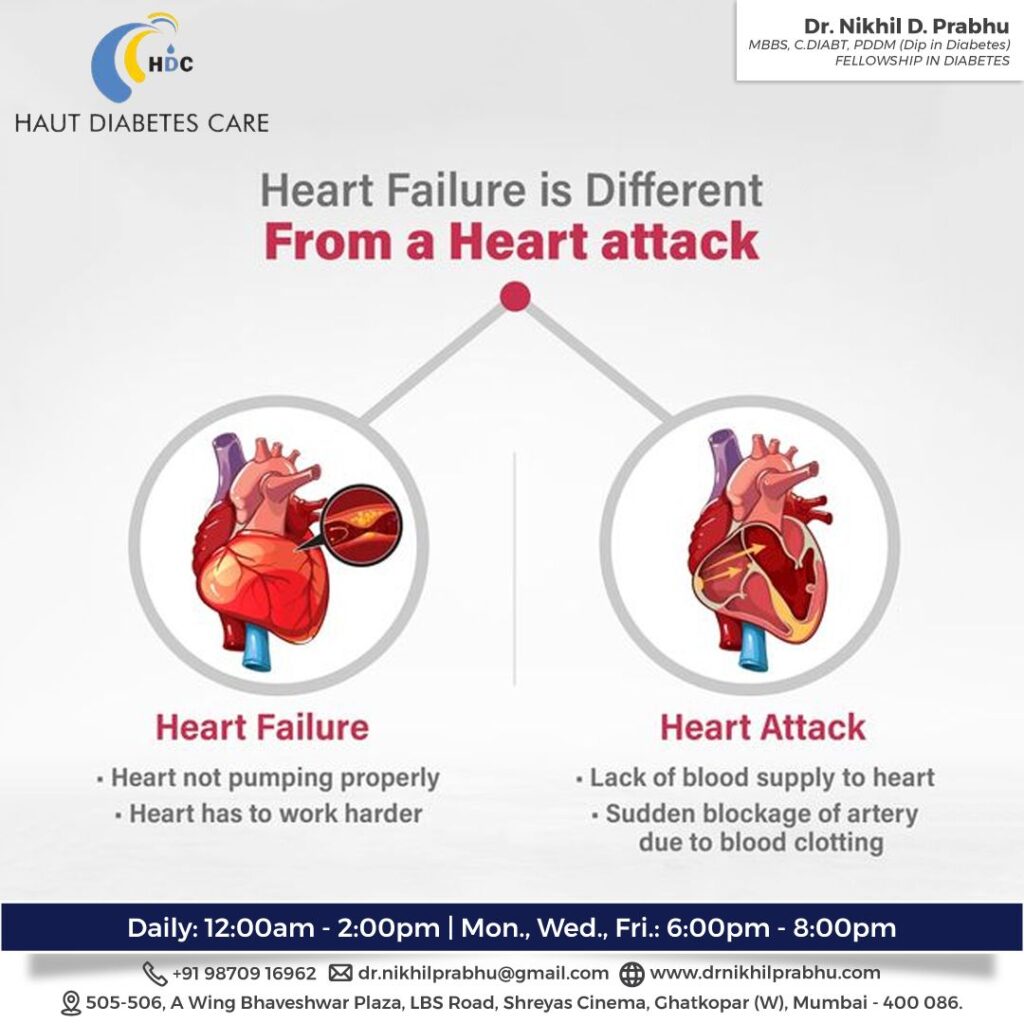
Heart failure and heart attack are two distinct medical conditions that affect the heart, but they differ in their causes, symptoms, and mechanisms. Here’s a comparison:
-
Causes:
- Heart Failure: Heart failure occurs when the heart’s pumping function becomes impaired, leading to the heart’s inability to effectively circulate blood and meet the body’s demands. It can be caused by various factors, including coronary artery disease, high blood pressure, heart valve disease, cardiomyopathy (disease of the heart muscle), congenital heart defects, and other conditions that affect the heart.
- Heart Attack: A heart attack, also known as myocardial infarction, happens when a coronary artery supplying blood to the heart muscle becomes blocked, usually by a blood clot. The blockage cuts off the blood supply to a portion of the heart muscle, resulting in tissue damage or death. The most common cause of a heart attack is the rupture or formation of a blood clot on a pre-existing atherosclerotic plaque in the coronary arteries.
-
Mechanism:
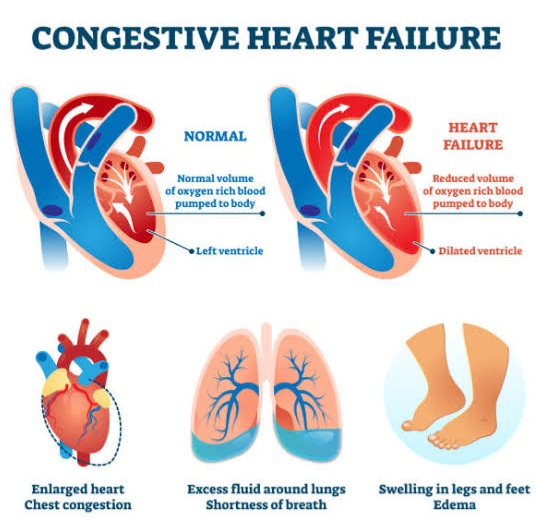
- Heart Failure: Heart failure refers to the heart’s inability to pump blood adequately, leading to a decrease in cardiac output. This reduced pumping efficiency can affect either the left side or the right side of the heart, or both. Heart failure often involves a combination of factors, such as weakened heart muscle, increased workload on the heart, or impaired relaxation and filling of the heart chambers.
- Heart Attack: A heart attack occurs due to the sudden interruption of blood flow to a part of the heart muscle. The blockage in a coronary artery deprives the heart muscle of oxygen and nutrients, leading to ischemia (lack of blood supply) and subsequent tissue damage. Prompt restoration of blood flow is crucial to prevent further injury to the heart muscle.
-
Symptoms:
- Heart Failure: The symptoms of heart failure can vary but often include shortness of breath, fatigue, swelling in the legs, ankles, or abdomen, rapid or irregular heartbeat, persistent cough or wheezing, reduced ability to exercise, and a feeling of congestion or fluid retention.
- Heart Attack: The symptoms of a heart attack commonly include chest pain or discomfort (which may radiate to the arm, neck, jaw, back, or stomach), shortness of breath, cold sweats, nausea, lightheadedness, and anxiety. However, it’s important to note that heart attacks can present differently in different individuals, and some may experience atypical symptoms or no symptoms at all.
-
Treatment:
- Heart Failure: The management of heart failure involves a combination of lifestyle changes, medications (e.g., diuretics, ACE inhibitors, beta-blockers), and, in some cases, interventions like cardiac resynchronization therapy, implantable devices (e.g., pacemakers, implantable cardioverter-defibrillators), or heart transplantation.
- Heart Attack: The immediate treatment for a heart attack involves restoring blood flow to the blocked coronary artery, typically through procedures such as angioplasty with stenting or thrombolytic therapy to dissolve the clot. Medications, such as antiplatelet drugs, anticoagulants, beta-blockers, and ACE inhibitors, are commonly prescribed to prevent further complications and manage the underlying causes.
In summary, heart failure refers to the heart’s inability to pump blood adequately, while a heart attack is caused by a blockage in a coronary artery. Although they can share similar symptoms, they have different causes, mechanisms, and treatment approaches. It’s important to consult with cardiologist & Diabetologist for accurate diagnosis, appropriate management, and individualized care.
Here are some more details about heart failure and heart attack:
Heart Failure:
- Types: Heart failure can be categorized into two main types: systolic heart failure and diastolic heart failure. Systolic heart failure occurs when the heart’s ability to contract and pump blood is weakened, whereas diastolic heart failure refers to the heart’s inability to relax and fill with blood properly.
- Stages: Heart failure is often classified into four stages based on the severity of symptoms and functional limitations. This classification system, called the New York Heart Association (NYHA) functional classification, ranges from Stage I (mild symptoms with no limitation of physical activity) to Stage IV (severe symptoms even at rest).
- Fluid Retention: One of the hallmark features of heart failure is fluid retention, leading to swelling in various parts of the body. This fluid buildup occurs because the heart’s pumping action is weakened, and blood can back up into the veins, causing congestion in organs such as the lungs, liver, and extremities.
- Complications: Heart failure can lead to various complications, including pulmonary edema (fluid accumulation in the lungs), arrhythmias (abnormal heart rhythms), kidney problems, liver dysfunction, and increased risk of blood clots.
Heart Attack:
- Types: Heart attacks can be classified based on the location and extent of the affected area. The most common type is a ST-segment elevation myocardial infarction (STEMI), which occurs when a complete blockage forms in a coronary artery. Non-ST-segment elevation myocardial infarctions (NSTEMIs) are less severe, as the blockage is usually partial or temporary.
- Ischemic Cascade: During a heart attack, the blockage in the coronary artery leads to a cascade of events known as the ischemic cascade. Initially, there is insufficient oxygen supply to the heart muscle, leading to ischemia. This causes the heart muscle cells to undergo injury and, if left untreated, can progress to irreversible damage (necrosis).
- Diagnosis: The diagnosis of a heart attack often involves a combination of clinical evaluation, electrocardiogram (ECG) to assess heart activity, blood tests (such as cardiac enzyme tests) to detect heart muscle damage, and imaging techniques like angiography or echocardiography to visualize the coronary arteries and assess heart function.
- Complications: Heart attacks can lead to several complications, including heart rhythm disturbances (arrhythmias), heart failure, cardiac arrest, cardiogenic shock (a state of inadequate blood supply to organs), and damage to other organs like the kidneys or brain.
It’s important to remember that while heart failure and heart attacks are distinct conditions, they can coexist or occur as a consequence of one another. For instance, a heart attack can lead to heart muscle damage and subsequently result in heart failure. Prompt medical attention and appropriate management are crucial for both conditions to improve outcomes and quality of life.
FAQ:
does heart failure cause heart attack ?
Heart failure itself does not directly cause a heart attack. However, the conditions that can lead to heart failure, such as coronary artery disease (CAD), can also increase the risk of a heart attack.
Coronary artery disease is a common cause of both heart failure and heart attacks. In CAD, the coronary arteries that supply blood to the heart muscle can become narrowed or blocked by the buildup of fatty plaques. This narrowing restricts blood flow to the heart, which can lead to symptoms of angina (chest pain) and an increased risk of heart attack.
If a coronary artery becomes completely blocked by a blood clot due to the rupture of a plaque, it can cause a heart attack. The blockage prevents oxygen-rich blood from reaching a portion of the heart muscle, leading to tissue damage or death in that area.
While heart failure and heart attacks can coexist, it’s important to note that heart failure is primarily a chronic condition resulting from the heart’s reduced ability to pump blood effectively, while a heart attack is an acute event caused by a sudden blockage of blood flow to the heart muscle. The presence of heart failure may increase the risk and severity of a heart attack, but it doesn’t directly cause a heart attack.