Difference between diabetes mellitus and insipidus?
Diabetes mellitus and diabetes insipidus are two distinct medical conditions, despite sharing the term “diabetes.” Here are the key differences between them:
Diabetes Mellitus:
Type 1 Diabetes: This type is usually diagnosed in children and young adults. It occurs when the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the body cannot produce insulin, leading to high blood sugar levels. Treatment typically involves insulin injections or the use of an insulin pump.
Type 2 Diabetes: This is more common and is often associated with lifestyle factors such as obesity and a sedentary lifestyle. In type 2 diabetes, the body’s cells become resistant to the effects of insulin, and the pancreas may not produce enough insulin. Management includes dietary changes, exercise, oral medications, and, in some cases, insulin.
Gestational Diabetes: Occurs during pregnancy and usually resolves after childbirth. It requires careful monitoring and may be managed with dietary changes and sometimes insulin.
High Blood Sugar: Diabetes mellitus results in high blood sugar levels (hyperglycemia) due to problems with insulin production or utilization.
Diabetes Insipidus:
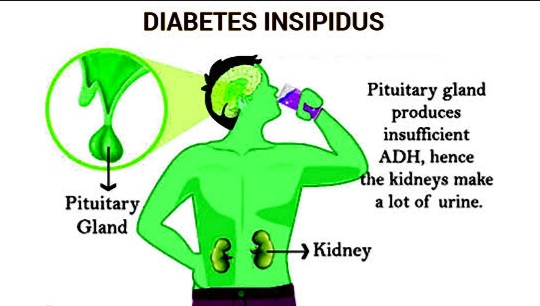
Central Diabetes Insipidus: This is caused by a lack of the hormone vasopressin (antidiuretic hormone) produced by the hypothalamus or released by the pituitary gland. Without vasopressin, the kidneys can’t properly regulate water balance, leading to excessive urination and thirst. It’s not related to blood sugar levels.
Nephrogenic Diabetes Insipidus: In this form, the kidneys do not respond properly to vasopressin, causing similar symptoms of excessive urination and thirst. This is usually due to a genetic condition or can be caused by certain medications.
Low Concentrated Urine: Diabetes insipidus leads to the production of large amounts of dilute urine (low urine concentration), as opposed to the high glucose levels in diabetes mellitus.
In summary, while both conditions involve increased urination and thirst, diabetes mellitus is related to problems with insulin and blood sugar regulation, whereas diabetes insipidus is related to the regulation of water balance and the antidiuretic hormone vasopressin. They have different causes, symptoms, and treatments.
Diabetes mellitus and diabetes insipidus are two different conditions that affect the body’s ability to regulate fluids and blood sugar levels.
Diabetes Mellitus:
Definition: Diabetes mellitus is a chronic metabolic disorder characterized by high blood sugar levels (hyperglycemia) resulting from the body’s inability to produce enough insulin or effectively use the insulin it produces.
Causes: Type 1 diabetes is caused by the immune system mistakenly attacking and destroying insulin-producing beta cells in the pancreas. Type 2 diabetes is usually caused by a combination of genetic and lifestyle factors, leading to insulin resistance and inadequate insulin production.
Symptoms: Symptoms of diabetes mellitus include increased thirst, frequent urination, unexplained weight loss, fatigue, blurred vision, and slow healing of wounds.
Treatment: Treatment for diabetes mellitus involves lifestyle modifications (such as diet and exercise) and, in many cases, medication like insulin injections or oral hypoglycemic drugs to manage blood sugar levels.
Diabetes Insipidus:
Definition: Diabetes insipidus is a rare disorder characterized by excessive thirst and urination. Unlike diabetes mellitus, diabetes insipidus is not related to blood sugar levels. It occurs when the kidneys are unable to properly concentrate urine, leading to large volumes of diluted urine.
Causes: Diabetes insipidus can be caused by a deficiency of antidiuretic hormone (ADH), also known as vasopressin, which regulates water reabsorption by the kidneys. This deficiency can result from damage to the hypothalamus or pituitary gland, or it can be a result of certain medications or kidney problems.
Symptoms: The main symptoms of diabetes insipidus are excessive thirst and urination, even at night, which can disrupt sleep. If left untreated, it can lead to dehydration and electrolyte imbalances.
Treatment: Treatment for diabetes insipidus typically involves replacing the deficient ADH with medications like desmopressin, which helps the kidneys reabsorb more water, reducing excessive urination and thirst.
In summary, diabetes mellitus is related to high blood sugar levels and insulin imbalance, while diabetes insipidus is characterized by excessive thirst and urination due to the inability of the kidneys to concentrate urine properly.